Onychomycosis, more commonly referred to as tinea unguium, is a highly contagious fungal infection of the nails. This is usually caused by a particular genus of fungi known as dermatophytes that thrive in the dead tissues of skin, nails, and hair. These fungi are typically able to proliferate at accelerated speeds by using potent enzymes to break down the dead tissue and colonise the area.
Onychomycosis can be transmitted through various means, from close contact with a person or animal who has the infection to visiting wet environments, like showers in gym locker rooms or public swimming pools. Additionally, use of contaminated objects, like nail clippers or files, can also facilitate the spread of the fungal growth.
Patients of onychomycosis might experience no indicators of the condition, but when symptoms do arise, they may include:
Fingernails can tell a story; discolored, thickened, brittle and/or ragged nails may be a warning sign of medical issues. In particular, observation of white or yellow pops on the nails raises a red-flag, as does experiencing pain or tenderness around the fingernail bed.
Left untreated, onychomycosis lurks the potential to be a contagious malady, morphing from nail-affecting to a full-blown skin infection encompassing the area around the nails. In cases of intense deterioration, this situation can become serious and escalate in severity.
An accurate diagnosis of onychomycosis involves a careful evaluation of the nails, as well as a test to confirm the presence of fungi. Tackling this fungal infection typically requires something more in-depth than just a topical solution – it may take several weeks or months of antifungal medications, both orally and topically.
Those with onychomycosis must be cautious in order to avoid re-infection. Basic hygiene is essential, particularly the keeping of nails clean and dry. Furthermore, nail clippers or nail files should never be exchanged with another person. Taking these steps will help ensure that the chance of re-infection remains low.
Related Product
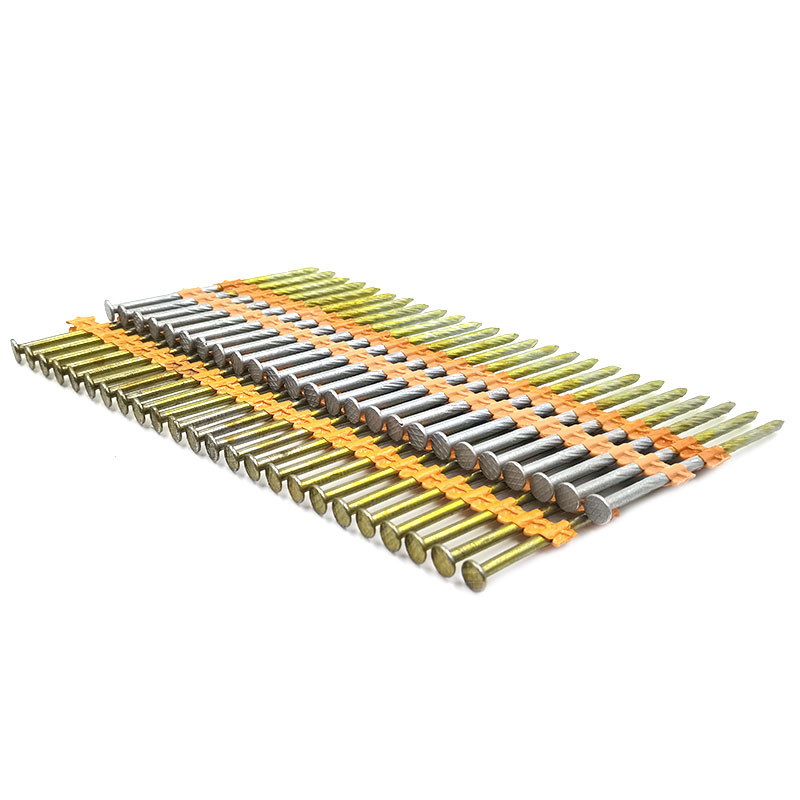
Plastic Strip Nail
Product Information: Diameter/mm(±0.05mm) Length/mm(±1.5mm) 2.87 50/60/65/70/75 3.05 70/75/83/90 3.33 75/83/90 3.76 75/90/100/130 4.11 75/90/100/130 4.5 75/90/100/130 Featur […]

Double Head Nail
Product Information: Material Q195/Q235 Surface Treatment Bright, E.G, H.D.G, M.G, V.C, C.C, P.C and so on Head Two Head Shank Smooth Shank Point Diamond Point Kinds of pa […]

Headless Nail
Product Information: Cheap Lost Head Nails/ Headless Nails/ Finishing Nails Price Material Q195 or Q235 iron wire rod or according to request Size 1″ – 6″ Finish Polished or […]

Concrete Nail
Product Information: Product name CONCRETE NAIL Material: #45 or #55 Steel Size: 1/2″-6″ Type: Round head with smooth shank or groove shank Treatment: Electro galvanized, ho […]

Shooting Nail
Product Information: GAS CONCRETE PIN NAIL raw material steel#45,#60 diameter 2.6mm,2.7mm,3.0mm,3.2mm length 13mm,16mm,19mm,22mm,27mm,32mm,37mm shank smooth shank & shri […]

Drywall Screw
Product Information: Product Name Screws Drywall Nail Material Carbon steel C1022a Color Black,Galvanized Standard ISO,GB,DIN,JIS,ANSI,BSW Diameter M3.5-M6.3, 6#-14# Length […]

U Sod Staple
Product Information: Landscape Staples * 11 GAUGE STEEL CONSTRUCTION: The points on the staples are sharp enough to pierce commercial ground cloth, and the staples are long […]

G Sod Staple
Product Information: Product name Sod Staple Material: Q195 /Q235 Size: 3/4X14GA, 3/4X9GA, 7/8X14GA, 1X9GA, 1-1/4X9GA, 1-1/2X9GA, 1-3/4X9GA Type: Round head with smooth shan […]

Fence U Nail
Product Information: U TYPE NAIL 1.material: Q195/Q235 Low Carbon Iron Rod 2.shank: smooth shank, single barbed shank, double barbed shank and others 3.Point: side cut point or di […]